What is it?
The Collaborative Bachelor of Science in Nursing is a joint partnership between the University of Windsor, St. Clair College and Lambton College.

A graduate of the FON’s BScN program at the U of W is an entry-to-practice practitioner who:
- Consistently demonstrates professional conduct in the provision of competent, ethical, compassionate, respectful, and culturally safe nursing care.
- Demonstrates accountability and responsibility for meeting professional practice expectations and learning needs.
- Minimizes harm and promotes healthy work environments by implementing strategies that promote patient, nurse, and environmental safety.
- Leads, follows, and manages to support and improve person/family, team, and organizational outcomes.
- Analyzes the impact of health care policy, finance, legal and regulatory environments on health care delivery.
- Applies the principles and skills of evidence-informed decision-making and quality improvement to promote optimal person/family and organizational outcomes.
- Applies clinical reasoning and knowledge-based practice to achieve optimal health outcomes for persons/families in stable and rapidly changing conditions and in diverse health care contexts (promotive, preventive, curative, rehabilitative, and end-of-life).
- Applies clinical judgement and decision-making when implementing procedures and interventions to ensure they are performed accurately, safely, efficiently, and compassionately in diverse health care environments.
- Coordinates care across settings and sectors of the healthcare continuum to address the changing care needs of persons, families, groups, communities, and populations.
- Educates persons/ families, groups, and communities to promote health across the spectrum of care.
- Actively engages in advocacy to promote social justice and health equity for persons, families, groups, communities and populations, and the nursing profession.
- Applies fundamental concepts of primary health care, health promotion, prevention, risk reduction, and the determinants of health across the lifespan.
- Applies and analyzes therapeutic relationships (person, family, groups) and communicates effectively (verbally, non-verbally, in writing).
- Collaborates effectively with persons/families, and within intra-professional and interprofessional teams to achieve optimal outcomes.
- Uses health informatics to develop, organize, deliver, and evaluate quality care in accordance with professional and regulatory standards.
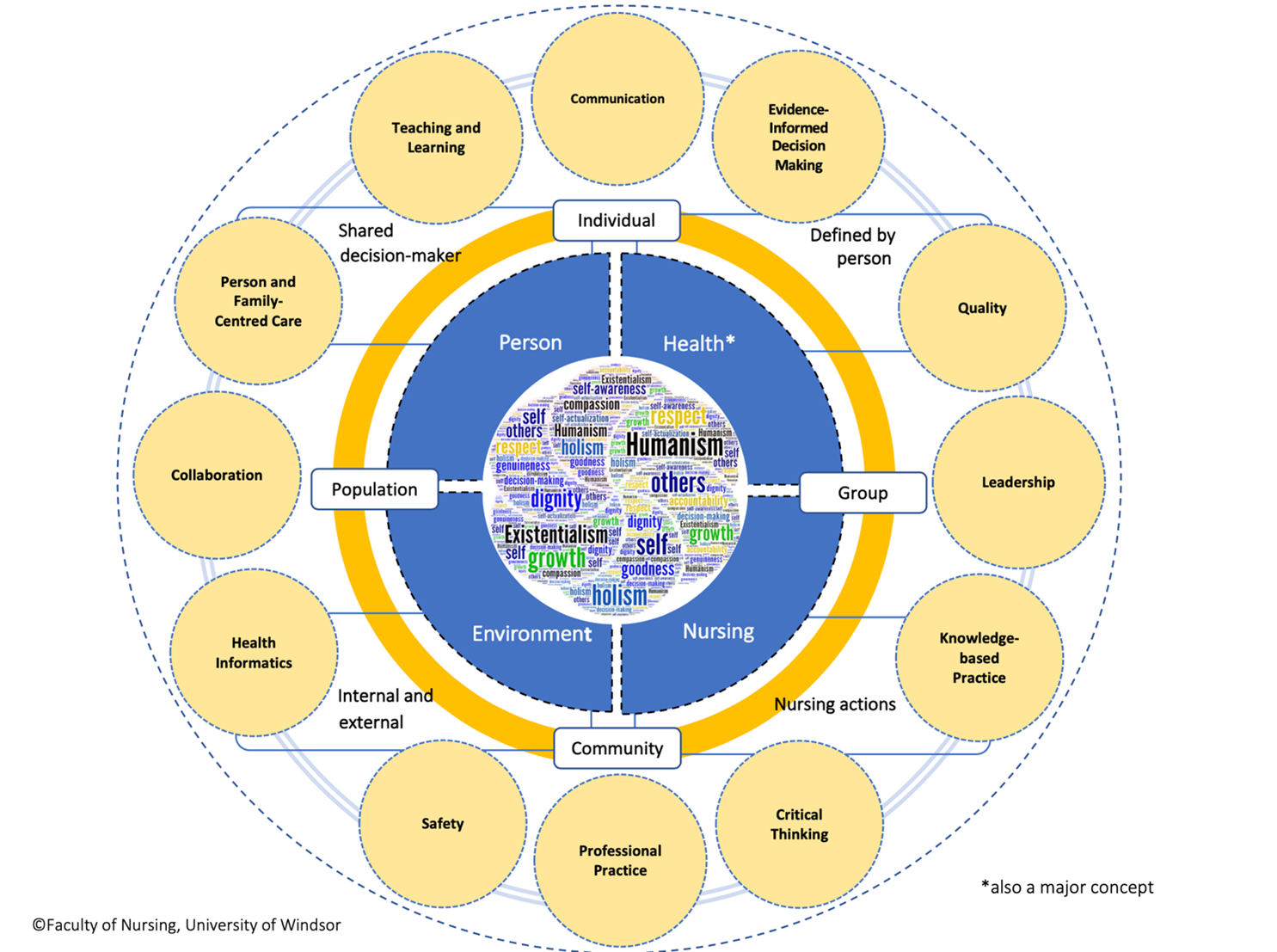
The BScN curriculum at the U of W is guided by a humanistic-existentialist philosophy.
A humanistic and existential philosophy emphasizes a person’s subjective experience as one of growth (Thomason, 2010). Growth is facilitated in self and others through attributes such as: dignity, genuineness, compassion, self-awareness, and self-responsibility. Healthy and meaningful interpersonal relationships support what is good and right and inform decisions that are in the best interests of self and others (Thomason, 2010), one’s community, and the nursing profession.
This philosophy informs our interpretation of the metaparadigm of nursing. The metaparadigm includes four constructs that are central to the discipline of nursing: person, health, environment, nursing (Fawcett, 1984), and our reflected in the following statements.
Person
Persons are holistic, unique, and multidimensional. Persons possess knowledge, have inherent dignity, and are worthy of respect. Persons are shared decision-makers who have capacity to enter reciprocal, caring, compassionate, and collaborative relationships that foster health and growth within and among individuals, families, groups, communities, and populations. All persons are autonomous. As such, persons are accountable and assume responsibility for their decisions and actions.
Health
Health is defined by the person. It is a dynamic process whereby the person, family, group, or community can realize aspirations, satisfy needs, and change or cope with the environment (World Health Organization, 1986). Health is a resource for everyday life and not just the absence of disease (World Health Organization, 1986). It emphasizes a person’s social and personal resources, as well as physical capacity. Health is the goal of all nursing behaviours (World Health Organization, 1986).
Environment
Environments are internal and external factors that influence health. Environments also include situations and settings within which individuals, families, groups, and communities strive to achieve optimal health by preventing disease and minimizing harm. Dynamic interpersonal interactions serve as a source of growth within these environments. Environments include internal and external factors and encompass psychosocial, cultural, spiritual, political, economic, and physical contexts that impact health and wellbeing within a care system.
Nursing
Nursing is a humanistic process, the goal of which is to help individuals, families, groups, communities, and populations achieve and maintain an optimal level of health consistent with their abilities, needs and desires. In collaboration with others, nurses use multiple actions to maximize individual, family, group, community, and populations strengths, to address health alterations, and to promote health and well-being. Nurses are responsible for promoting growth and goodness in others, the community, populations, and the nursing profession.
Thirteen major concepts guide the BScN curriculum. They are congruent with the FON’s philosophy and are organized around the metaparadigm of nursing constructs. These core concepts were selected after a comprehensive review of the current state of the BScN program at the U of W, and the future direction of nursing education and practice in Canada and around the world. These concepts (and their related sub-concepts) and are not mutually exclusive, but rather applied in combination. They reflect the processes/activities through which our interpretation of the metaparadigm is enacted.
- Critical thinking
- Knowledge-based practice
- Evidence-informed decision making
- Health
- Teaching and learning
- Professional practice
- Communication
- Leadership
- Collaboration
- Quality
- Safety
- Person family-centered care
- Health informatics
Refer to Figure 1 for a depiction of the Conceptual Model.
Each concept is defined and levelled within the U of W’s BScN curriculum to prepare graduates to practice in multiple contexts and settings, with individuals, groups, communities and populations. Their synergistic organization enables student achievement of the FON’s BScN Program Outcomes and reflects the program philosophy.
Figure 1. Program Model
|
Major Concepts and Definitions |
Sub-Concepts and Definitions |
|
|---|---|---|
|
1.0 Critical Thinking
Definition: “a disciplined and systematic process that is based on the ability to collect data, reflect on the data collected, and make appropriate conclusions and/or decisions” (Taylor et al., 2011).
The “ability to apply higher-order cognitive skills (conceptualization, analysis, evaluation) and the disposition to be deliberate about thinking (being open-minded or intellectually honest) that lead to action that is logical and appropriate” (Papp et al. 2014, p. 716).
|
Clinical reasoning
|
A logical process by which nurses make clinical judgments by collecting cues, processing the information, understanding the problem/situation, selecting and implementing interventions based on the evidence and by intuition and pattern recognition, then evaluating the outcomes and reflecting on the process (Hoffman, 2007; Tanner, 2006). It involves use of the nursing process and diagnostic reasoning. |
|
Clinical judgment
|
An interpretation or conclusion about a person’s needs, concerns, or health problems, and/or the decision to take action (or not), use or modify standard approaches, or improvise new ones as deemed appropriate by the person’s response (Tanner, 2006). |
|
|
Decision-making
|
The ability to draw on many modes of thinking in order to select a course of action. It involves understanding and anticipating risks, benefits and outcomes beyond what is obvious, and creating a proactive plan of action based on this analysis (CNO, 2014) |
|
|
Systems thinking |
An approach to problem solving that views problems as part of a system. It can be applied to decode the linkages and components within a health system, and then applies the understanding to design and evaluate interventions that maximize health and health equity (WHO, 2009) |
|
|
2.0 Knowledge-Based Practice
Definition: composed of foundational and in-depth theoretical, conceptual and factual content (diverse sources of knowledge and ways of knowing, including theories and nursing knowledge from the sciences, humanities, research, ethics, culture, and spirituality) and the application of this knowledge in competent practice (CASN 2015; CNO 2009) |
Includes integration of learner outcomes from all courses that support the acquisition and application of a specialized body of knowledge and the competent application of this knowledge Examples: fundamentals of care, technical procedures, pharmacology, medication management, nutrition, anatomy and physiology, microbiology, biochemistry |
|
|
3.0 Evidence-Informed Decision-Making
Definition: Integrating the best research evidence with personal preferences, while considering the clinical setting, health care resources, and clinical expertise to make decisions about programs, practices or policies (Haynes, 2007; McMaster University).
|
Evidence-based nursing
|
"An ongoing process by which evidence, nursing theory and the practitioners’ clinical expertise are critically evaluated and considered, in conjunction with patient involvement, to provide delivery of optimum nursing care for the individual" (Scott & McSherry, 2009) |
|
Information literacy
|
“The ability to recognize when information is needed and have the ability to locate, evaluate, and use the information efficiently…It is common to all disciplines, and supports lifelong learning. It enables learners to master content and extend their investigations, become more self-directed, and assume greater control over their own learning (McMaster University, 2017). |
|
|
4.0 Health
Definition: A multidimensional concept that is not the absence of disease or illness but rather "the extent to which an individual or group is able to realize aspirations and satisfy needs, and to change or cope with the environment. It is a resource for everyday life, not the objective of living; it is a positive concept, emphasizing social and personal resources, as well as physical capacities" (WHO, 1984). Health exists on a continuum and encompasses the entire life span beginning with birth and including palliative care and ending in death (Arnold, 2011).
|
Health promotion |
“The process of enabling people to increase control over, and to improve, their health. It moves beyond a focus on individual behaviour towards a wide range of social and environmental interventions” (World Health Organization, 2017). |
|
Disease prevention
|
"Specific, population-based and individual-based interventions for primary and secondary prevention, aiming to minimize the burden of diseases and associated risk factors" (WHO, 2017). Related sub-concept harm reduction. |
|
|
Population health |
An approach to health that aims to improve the health of the entire population and to reduce health inequities among population groups. It looks at and acts upon the broad range of factors and conditions that have a strong influence on health (PHAC, 2012) |
|
|
Primary health care |
A comprehensive approach to health care delivery that is integral to improving health across the continuum of care (birth to death) and in all care settings. It puts the people who receive those services at the centre of care. The essential principles are: accessibility, active public participation, health promotion and chronic disease prevention and management, use of appropriate technology and innovation, and intersectoral cooperation and collaboration (CNA, 2017). |
|
|
Social determinants of health
|
“The conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels” (WHO, 2017). They include: income and social status, social support networks, education and literacy, employment and working conditions, social environments, physical environments, personal health practices and coping skills, healthy child development, biology and genetic endowment, health services, gender, culture (PHAC, 2012). |
|
|
Health literacy
|
“The degree to which an individual has the capacity to obtain, communicate, process, and understand basic health information and services to make appropriate health decisions” (U.S. Department of Health and Human Services, 2000).
“The cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health” (WHO, 2017).
|
|
|
Health equity
|
Differences in health associated with social disadvantages that are modifiable, and considered unfair; all people (individuals, groups and communities) have a fair chance to reach their full health potential and are not disadvantaged by social, economic and environmental conditions (NCCDH, 2014). |
|
|
5.0 Teaching and Learning
Definition: Teaching is a purposeful activity that facilitates learning. Teaching and learning are shared and reciprocal processes that are based on past experiences. Learning is evidenced by a change in knowledge, skill, behaviour, perception, insight, and/or attitude. Learning continues across one's lifetime (Prozesky, 2000)
|
|
|
|
6.0 Professional Practice
Definition: Encompasses all aspects of professional conduct, including accountability for meeting learning requirements, responsibility for one’s actions, and respect for others. Includes knowledge of the healthcare system to provide foundation to support and/or advocate for policy and system changes.
|
Accountability
|
The ability and willingness to assume responsibility for one’s own actions (RNAO, 2007). It involves knowing and understanding the roles and responsibilities of other team members, collaborating, consulting and taking action on client information when needed, taking action to ensure client safety, including informing others about concerns related to the conduct and/or actions of other care providers, and collaborating with clients, with each other and with members of the interprofessional care team for the benefit of the client (CNO, 2014). |
|
Responsibility |
Acting according to organizational and professional codes of conduct and standards of practice. |
|
|
Continuing competence |
The ability to use one’s knowledge, skill, judgment, attitudes, values and beliefs to perform in a role, situation and practice setting and perform in a changing health care environment. |
|
|
Ethics
|
“A system of valued behaviours and beliefs for determining right or wrong and for making judgments about what should be done to or for other human beings”
“Nursing ethics is reasoned reflection and enquiry about the ethical dimensions of nursing practice as it impacts on the lives of patients, colleagues, and society” (RNAO, 2007) |
|
|
Law
|
The set of provincial and federal laws that govern healthcare and regulate the practice of registered nurses (e.g. Canada Health Act, Regulated Health Professions Act, The Nursing Act, Health Care Consent Act etc.) |
|
|
Self-regulation |
The ability of a profession to predominantly control its own admission standards and requirements and the practice norms for its practice by recognizing that the profession itself is best qualified and situated to define its practice and boundaries by identifying, implementing, monitoring and addressing deviation from its own standards of education, its practices and its own articulated professional ethics framework (CNA, 2006) |
|
|
Advocacy |
Supporting and/or speaking out for a cause or policy. It includes being an advocate/change agent for clients, families and communities and the profession (RNAO, 2007). |
|
|
Social justice |
“The fair distribution of resources and responsibilities among members of a population with a focus on the relative position of one social group compared to to others, and on the root causes of disparities and strategies for their elimination (CNA, 2006).
|
|
|
Cultural care |
Nursing practice that recognizes the shared patterns and learned values and behaviours of groups that are transmitted over time (CNA, 2004), and that responds appropriately to address the client's cultural expectations and needs. It is a component of quality practice environments that leads to improved health outcomes for clients, nurses and systems (CNA, 2009). Related sub-concepts include cultural awareness, cultural sensitivity, cultural competence and cultural safety. |
|
|
7.0 Communication
Definition: An active, transactional, purposeful, multidimensional, and irreversible process that is guided by conscious participation with patients/clients and health care providers using relational practices and skills. (CRNBC, 2014). It combines the integration of verbal nonverbal, and written behaviours (Arnold and Boggs, 2017; Hargie, 2011). It includes therapeutic nurse-client relationships, counselling, and professional communication.
|
Therapeutic relationship
|
A relationship within which the client’s needs are the focus and which is based on trust, respect, intimacy, mutuality, reciprocity, reflection and the appropriate use of power. It involves empathy and caring (CNO, 2002) |
|
Counselling
|
A direct care method and empowerment approach that helps people (individuals, families, groups) to use problem-solving methods to recognize health needs, examine alternative interventions and decide which are useful and appropriate (Potter, 2011).
|
|
|
Professional communication
|
Includes all elements of communication that establish and convey trustworthiness and competence in a variety of interactions (interpersonal, transpersonal, group, public) and that includes professional appearance, attitude, and behaviours (Goddard, 2011).
|
|
|
8.0 Leadership
Definition: A relational process in which an individual seeks to influence others towards a mutually desirable goal (RNAO, 2013). As cited in CNO glossary
Leadership is not a trait but a set of capabilities that prepare a nursing student to influence others to achieve an outcome. Nurses can lead at the micro-level (e.g., working with individuals and teams), at the meso-level (e.g., developing organizational policies), and at the macro-level (e.g., enacting change at the national level) (Gallagher, 2010). The five practices of exemplary leaders (Kouzes and Posner) prepare students to: model the way (responsibility for personal behaviour), inspire a shared vision, challenge the process, enable others to act, and encourage the heart (empathy, productive relationships). |
Followership
|
Followership is a role. It is the ability of an individual to follow a leader (Riggio et al., 2008). It involves “engaging with others who are leading or managing by contributing to problem identification, completing tasks, and providing feedback for evaluation” (Yoder-Wise, 2011, p. 6). Effective followers demonstrate self-management, commitment, competence and focus and courage (Kelley, 1988). Both effective leadership and followership are required to accomplish organizational goals and quality outcomes. |
|
Management
|
The coordination and integration of resources through planning, organizing, coordinating, directing, and controlling to accomplish specific organizational goals and objectives (Huber, 2010) |
|
|
Care coordination |
All RNs play a role in coordination of care for persons/families. Specialized roles and models are emerging in all settings (e.g., case managers, nurse navigators, disease management). Care coordination is focused on ensuring that the person’s needs/ preferences are planned with respect to health services and information is shared across providers and sites to facilitate the appropriate delivery of health care services.
|
|
|
9.0 Collaboration
Definition: A solution-oriented process of working together to solve a problem. It involves having common goals, open communication, mutual trust, shared decision making and role clarity (Boggs, 2016)
|
Teamwork
|
“A dynamic process involving two or more healthcare professionals with complementary backgrounds and skills, sharing common health goals and exercising concerted physical and mental effort in assessing, planning, or evaluating patient care. This is accomplished through interdependent collaboration, open communication and shared decision-making, and generates value-added patient, organizational and staff outcomes”(Xyrichis & Ream, 2008) |
|
Inter-professional
|
"When multiple health workers from different professional backgrounds work together with patients, families, carers (caregivers), and communities to deliver the highest quality of care" (WHO, 2010). |
|
|
Intra-professional
|
Multiple members of the same profession working together to deliver quality care (CNO, 2014). |
|
|
10.0 Quality
Definition: The six dimensions of quality include: safe (avoiding injuries to patients from the care that is intended to help them), effective (providing services based on scientific knowledge to all who could benefit, and refraining from providing services to those not likely to benefit), patient-centred (providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions), timely (reducing waits and sometimes harmful delays for both those who receive and those who give care), efficient(avoiding waste, including waste of equipment, supplies, ideas, and energy), equitable (providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status). (IOM, Crossing the Quality Chasm, 2003) |
Quality improvement/ improvement science |
Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems (QSEN, 2007).
“A broad range of activities of varying degrees of complexity and methodological and statistical rigour through which healthcare providers develop, implement and assess small-scale interventions, identify those that work well and implement them more broadly in order to improve clinical practice” (The Ethics of Improving Health Care Quality & Safety: A Hastings Center/AHRQ Project, Mary Ann Baily, PhD, Associate for Ethics & Health Policy, The Hastings Center, Garrison, New York, October, 2004). |
|
11.0 Safety
Definition: Minimizes risk of harm to patients and providers through both system effectiveness and individual performance (QSEN, 2007)
|
Patient safety
|
The pursuit of the reduction and mitigation of unsafe acts within the health care system, as well as the use of best practices shown to lead to optimal patient outcomes (CPSI, 2008; 2009). Includes creation of a culture of safety. |
|
Nurse and environmental safety |
The use of best practices to reduce the hazards in practice environments: biological, chemical, psychological, physical hazards and violence (aggression, harassment, bullying, intimidation and assault). |
|
|
12.0 Person-Family Centred Care
Definition: A partnership between a team of health providers and an individual where the person retains control over his/her care and is provided access to the knowledge and skills of team members to arrive at a realistic team shared plan of care and access to the resources to achieve the plan (Orchard, 2008). It has two overarching values: dignity and respect, and it involves four processes: information sharing, partnership, participation, and collaboration. Source: http://www.ipfcc.org/about/pfcc.html
|
|
|
|
13.0 Health informatics
Definition: A science and practice [which] integrates and manages information and knowledge and communication technologies to promote the health of people, families and communities worldwide (CASN, 2012) |
Information and communication technologies |
Encompasses all those digital and analogue technologies that facilitate the capturing, processing, storage, and exchange of information via electronic communication. |
|
Health Information Systems |
A combination of vital and health statistical data from multiple sources, used to derive information and make decisions about the health needs, health resources, costs, use, and outcome of health care. |
|
|
Nursing informatics |
A science and practice [which] integrates nursing, its information and knowledge, and their management, with information and communication technologies to promote the health of people, families and communities worldwide. |
|
